Need Help?
Ask an expert
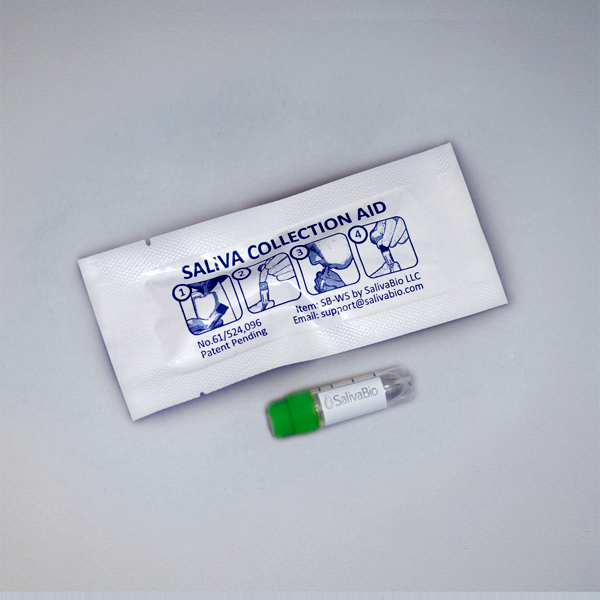
1. How to collect Salivary Insulin
APPROVED SALIVARY INSULIN COLLECTION METHODS
Salivary Insulin Collection Protocol
Collection volume, general considerations, and basic guidelines to maximize salivary insulin sample integrity. Use this analyte-specific collection protocol to plan you collection methodology and sampling schemes.
2. How to Assay for Salivary Insulin
Send Saliva Samples to Salimetrics
Add to StudyEasy and accurate results from the most trusted Salivary Bioscience Laboratory.
All Lab ServicesOrder Code5452
3. Technical Summary
| Analyte Summary | |
|---|---|
| Analyte: | Insulin |
| Aliases: | INS, IDDM, IDDM1, IDDM2, ILPR, IRDN, MODY10 |
| Serum-Saliva Correlation: | 0.92 |
| *Optimum Collection Volume: | 100 μL |
| Special Considerations |
|---|
| Fasting Insulin: Do not consume food or beverage within eight hours prior to saliva collection. Glucose Challenge: Salivary insulin levels lag approximately 1 hour behind blood levels. |
| Assay Summary | |
|---|---|
| Methodology: | ELISA |
| Sensitivity: | 7.5 pg/mL |
| Assay Range: | 3.2-50,000 pg/mL |
| Assay Type: | Quantitative |
Background
Insulin, a core anabolic peptide hormone, is responsible for regulating the metabolism of nutrients such as glucose and fatty acids to promote their absorption into fat, liver, and skeletal muscle cells. It also suppresses the breakdown of proteins into amino acids. Circulating insulin levels stimulate cellular glucose oxidation, glycogenesis, lipogenesis, and proteogenesis to maintain glucose homeostasis and are mainly modulated by beta cells in the islets of Langerhans and hyperglycemic hormones such as cortisol, glucagon and growth hormones. Multiple systems, as well as metabolic and neural influences co-function to regulate insulin levels. Prolonged deficiencies in insulin regulation have been linked to a myriad of health risks, including metabolic syndrome, obesity, diabetes mellitus, water bloating, high blood pressure, endocrine dysfunctions and increased levels of inflammatory compounds in the blood. In saliva, insulin shares a near linear correlation to fasting blood levels and is a reliable surrogate for serum measures, with a 0.92 correlation (Fabre 2012). During an oral glucose tolerance test, research shows a ~30 minute delay between salivary insulin and the spike in serum insulin levels (Fekete 1993). Overall, salivary insulin presents a unique opportunity to monitor insulin levels prior to disease progression. Elevated fasting insulin is a hallmark of insulin resistance, which can precede type 2 diabetes onset by several years and may be used to justify changes in lifestyle to reduce the risk of disease (Tomoshige Hayashi 2013).
References & Salivary Insulin Research
- Goodson, JM, et al. (2014). Metabolic Disease Risk in Children by Salivary Biomarker Analysis. PLoS One. 9(6): e98799.
- Fekete Z, et al. (1993). Salivary and plasma insulin levels in man. Biochem Mol Biol Int. 30(4): 623–629.
- Fabre B, et al. (2012). Measurement of fasting salivary insulin and its relationship with serum insulin in children. Endocr Connect. 1(2): 58–61.
- Hartman ML, et al. (2016). Unhealthy Phenotype as Indicated by Salivary Biomarkers: Glucose, Insulin, VEGF-A, and IL-12p70 in Obese Kuwaiti Adolescents. J Obes. 2016: 6860240.
- Ebbeling CB, et al. (2002). Childhood obesity: public-health crisis, common sense cure. Lancet. 360(9331):473-82.
- Zhao X, et al. (2016). Using Metabolomic Profiles as Biomarkers for Insulin Resistance in Childhood Obesity: A Systematic Review. J Diabetes Res. 2016:8160545.
- D’Adamo E, et al. (2011). Type 2 diabetes in youth: epidemiology and pathophysiology. Diabetes Care. 34 Suppl 2:S161-5.
- Hayashi T, et al. (2013). Patterns of Insulin Concentration During the OGTT Predict the Risk of Type 2 Diabetes in Japanese Americans. Diabetes. 36(5): 1229-1235.
 Contact: Salimetrics (USA)
Contact: Salimetrics (USA)